Anal fistulas are abnormal tunnels that form between the anal canal and the skin near the anus. They often develop after an infection in the anal glands that creates an abscess. While mild cases may be managed with medications, including antibiotics and anti-inflammatory treatments, not all fistulas respond to these conservative approaches. Chronic or complex fistulas tend to resist medication, causing recurring infections, pain, and drainage. Understanding the reasons behind medication failure is essential for determining the next steps in treatment. Many patients are surprised to learn that relying solely on medications may not fully resolve the underlying problem. When infections keep returning, and symptoms persist, surgical solutions become the most effective path to long-term healing.
Medication may fail due to the complex nature of the fistula or the presence of multiple tracts that are not fully accessible by antibiotics. Patients with chronic conditions such as Crohn’s disease may experience higher resistance to non-surgical treatments. Additionally, poor blood flow or immune system weaknesses can prevent medications from effectively targeting the infection. Recurrent abscesses and persistent discomfort are common signs that a more definitive solution is required. Even lifestyle adjustments like diet modification or hygiene measures sometimes fall short when the fistula is extensive or deep. Understanding these limitations helps patients make informed decisions about surgical interventions. The shift from medical to surgical treatment is often a turning point in effectively managing anal fistulas.
Signs That Indicate the Need for Surgical Intervention
Persistent pain or swelling around the anal area is one of the most apparent signals that surgery may be necessary. Patients often experience continuous discharge or foul-smelling drainage that does not respond to medications. Recurrent infections despite rigorous antibiotic therapy are another key indicator. Difficulty managing symptoms through conservative measures can significantly impact daily life, including sitting, walking, and working. Advanced imaging techniques like MRI or endoscopic evaluation are used to assess the severity and structure of the fistula. Physical examination by a specialist can reveal multiple tracts or hidden abscesses that contribute to persistent problems. When these signs are present, surgical solutions provide a reliable path to both symptom relief and long-term healing.
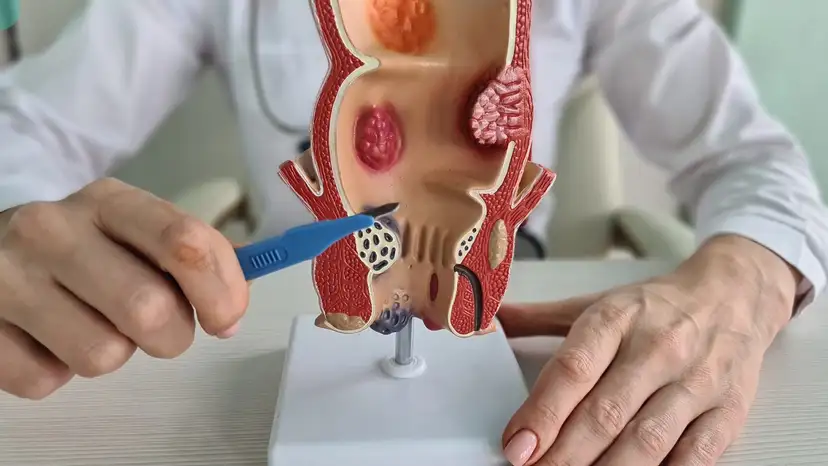
Overview of Surgical Options for Anal Fistulas
Surgery aims to eliminate the fistula, prevent infection, and preserve the function of the anal sphincter. Several surgical techniques are commonly used, each tailored to the fistula’s complexity and location.
- Fistulotomy involves opening the fistula tract to allow healing from the inside out. It is commonly used for simple fistulas with a single tract.
- Fistulectomy removes the entire fistula tract, reducing the risk of recurrence but requiring careful management of surrounding tissue.
- Seton Placement uses a surgical thread to drain the fistula gradually and encourage healing over time. This technique is often applied to complex or high fistulas.
- Advancement Flap Procedure repairs the internal opening while protecting the sphincter, making it ideal for preserving continence in complicated cases.
- LIFT Procedure (Ligation of Intersphincteric Fistula Tract) is minimally invasive, targeting the fistula tract while sparing the sphincter muscles.
Comparing these procedures, patients should consider factors like recovery time, potential complications, and long-term effectiveness. A qualified surgeon will recommend the best option based on the fistula’s complexity, the patient’s health, and previous treatments. Understanding the range of surgical solutions helps patients feel empowered and prepared for what to expect.
Preparing for Anal Fistula Surgery
Proper preparation before surgery significantly improves outcomes and reduces the risk of complications. Pre-operative consultations allow the surgeon to evaluate the fistula using imaging and physical examination. Patients are often advised to follow specific bowel prep protocols to reduce infection risk. Maintaining proper hygiene and following dietary recommendations can aid in smoother recovery. Discussing expectations with the surgeon ensures that the patient understands the procedure, recovery timeline, and possible side effects. Some lifestyle adjustments may be necessary, such as temporarily avoiding heavy lifting or strenuous exercise. Psychological preparation is equally important, as understanding the process can reduce anxiety and improve post-operative compliance.
Recovery and Post-Surgical Care
Recovery after anal fistula surgery requires attention, patience, and proper care. Patients usually experience mild to moderate discomfort, which can be managed with prescribed pain medications. Regular cleaning and dressing of the surgical site are essential to prevent infection and promote healing. Maintaining a high-fiber diet and staying hydrated helps prevent constipation, which is critical for avoiding strain on the healing tissue. Activity restrictions may include avoiding prolonged sitting or heavy lifting for several weeks. Close follow-up appointments allow the surgeon to monitor healing, remove sutures if necessary, and identify any early signs of recurrence. Awareness of potential complications, such as infection or incontinence, ensures that issues can be addressed promptly.
Long-Term Management and Prevention
Even after successful surgical repair, long-term management is key to preventing recurrence. Regular check-ups allow the surgeon to monitor the site for any signs of new fistula formation. Maintaining gut and anal health through a balanced diet, adequate hydration, and consistent bowel habits supports tissue recovery. Avoiding smoking and managing chronic conditions like Crohn’s disease can further reduce the risk of recurrence. Patients should be aware of warning signs, such as persistent pain, swelling, or drainage, and seek prompt medical attention if these occur. Integrating lifestyle habits that support digestive health helps sustain the benefits of surgery. Educating patients on long-term care empowers them to take active roles in their recovery.
Frequently Asked Questions
- How long does it take to recover from anal fistula surgery? Recovery typically ranges from 4 to 8 weeks, depending on the procedure’s complexity.
- Are there risks of incontinence after surgery? Some procedures carry a small risk, but techniques like the LIFT or advancement flap minimize this risk.
- Can anal fistulas recur after surgical repair? Recurrence is possible, especially with complex fistulas, but proper surgical technique reduces the likelihood.
- How painful is the recovery period? Pain varies but is usually manageable with prescribed medications and proper wound care.
- Is it possible to return to work soon after surgery? Many patients can resume light duties within a week or two, but physically demanding work may require more time.
- Are minimally invasive procedures as effective as traditional surgery? For select cases, minimally invasive techniques offer similar success with faster recovery.
- Can lifestyle changes prevent recurrence? Yes, a high-fiber diet, hydration, proper hygiene, and management of underlying conditions support long-term results.
Takeaway
When medication fails, surgical solutions for anal fistulas provide a definitive path to relief and healing. Understanding the signs that indicate surgery, knowing the available procedures, and preparing properly for both surgery and recovery can greatly enhance outcomes. Long-term management and lifestyle adjustments play a crucial role in maintaining anal health and preventing recurrence. Working closely with a specialist ensures that each patient receives a personalized treatment plan, addressing both the physical and emotional aspects of this condition. Surgical repair is not just a procedure—it is a step toward reclaiming comfort, function, and quality of life.